
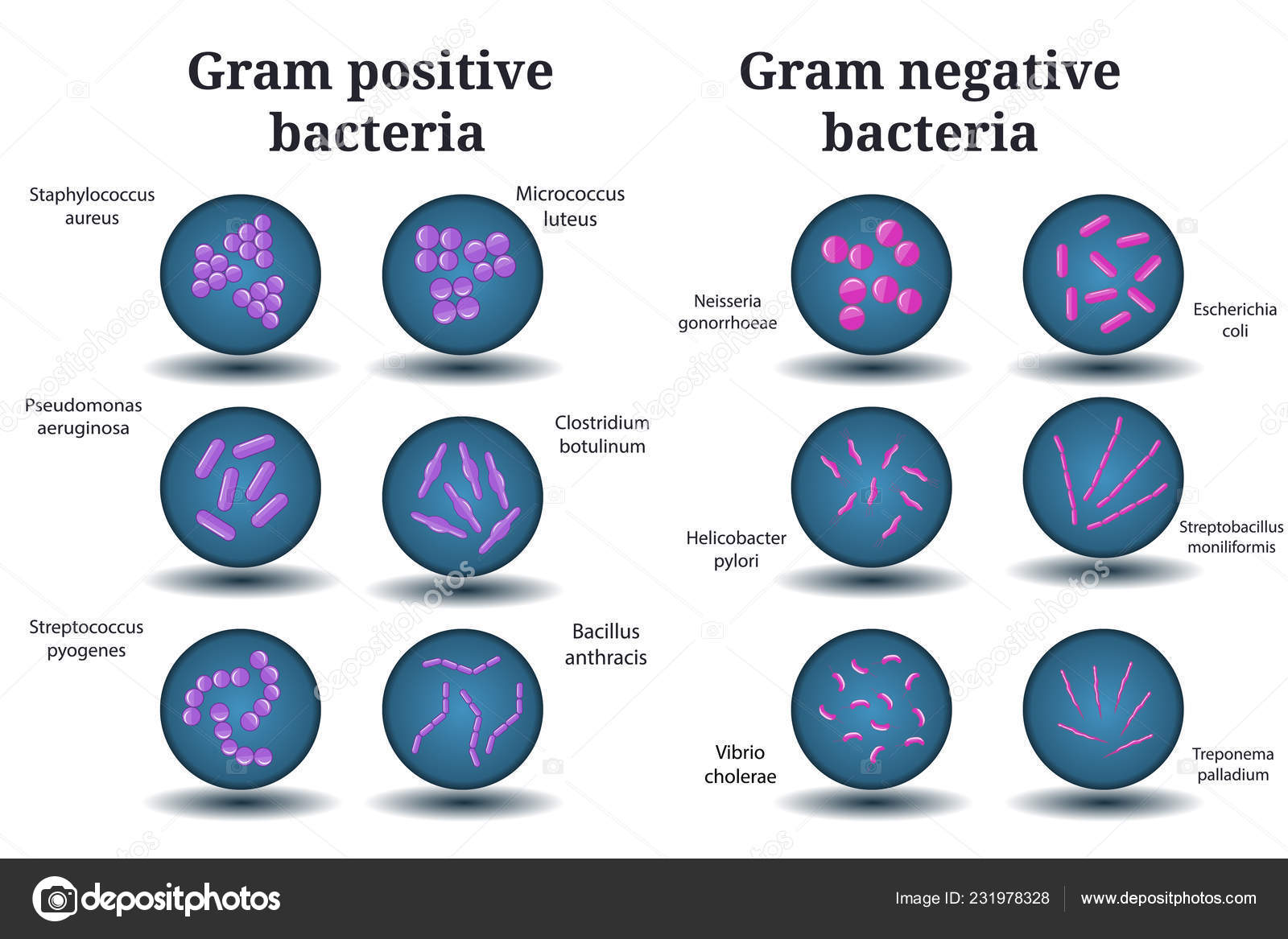
This includes plans to reduce the number of healthcare associated Gram-negative bloodstream infections by 50%, by financial year 2020 to 2021. In November 2016, the government announced plans to reduce infections across the NHS. Use the enhanced surveillance form to report mandatory surveillance of Gram-negative bacteria. Read NHS Improvement’s ambition to halve healthcare associated Gram-negative bloodstream infections Submit data Guidance on preventing healthcare associated Gram-negative bacterial bloodstream infections is available from the NHS Improvement website. Some of the antibiotic resistance mechanisms are on mobile genetic elements, such as plasmids, which allow the genes that encode resistance to spread more easily, and importantly, between different bacterial species. Gram-negative bacteria can be resistant to antibiotics and in some cases will be multi-resistant rendering most available antibiotics useless. and Pseudomonas aeruginosa are the leading causes of healthcare associated bloodstream infections. Gram-negative bacteria such as Escherichia coli, Klebsiella spp. One of the most serious infections Gram-negatives can cause bloodstream infections. Some live in the intestine harmlessly, while others may cause a variety of diseases.īacteria that are normally harmless in their normal environment can cause problems if they grow in other parts of the body and can cause a range of infections with differing severity and associated mortality. There are many different types of Gram-negative bacteria.


 0 kommentar(er)
0 kommentar(er)
